205
Surgery in AMD
limited macular translocation is associated with addi-
tional risks similar to those of scleral buckling surgery.
As with full macular translocation, the rate of compli-
cations won its popularity. Although conceived in an
effort to reduce the rate of PVR development, this has
remained the most common serious complication after
limited macular translocation. Rates of retinal detach-
ment up to 17.4% have been reported
(29)
. Insufficient
macular translocation is another important limitation
of this procedure, restricting its indications to smaller
CNV.
Is there a role for macular translocation in the current
era of anti-VEGF therapy and combined treatments?
In the latest edition of
Vitreous Microsurgery (4th Edition,
2007 - Lippincott Williams &Wilkins)
(20)
, Steve Charles
et al. stated that, at the present time, macular trans-
location has no place in the treatment of age-related
macular degeneration. They argued that these proce-
dures still come with an unacceptable number of serious
complications.
In a recent review of the functional outcomes of macu-
lar translocation for wet-AMD, Eandi et al.
(30)
concluded
that there wasn’t enough evidence in randomized trials
to support the benefit of surgery. Future studies should
involve patients with small neovascular membranes that
are non-responsive to the present medical armamentar-
ium, and that accept the risks of surgery in an effort to
improve their visual function.
This is essentially a five-step procedure, that starts with
the placement of scleral imbricating sutures (either in
the superotemporal or inferotemporal quadrants for
inferior and superior translocations, respectively) for
antero-posterior shortening of the eyewall. This is fol-
lowed by a pars plana vitrectomy with posterior vitreous
detachment induction. The third step should be an inter-
nal subretinal hydrodissection through small self-sealing
retinotomies for creation of a partial neurosensory reti-
nal detachment. After tightening the scleral imbricating
sutures, a redundancy of the neurosensory retina relative
to the eyewall is created that should allow the desired
foveal displacement, after retinal reattachment with
fluid-air exchange. Limited macular translocation may
be either inferior or superior, depending on the move-
ment of the neurosensory macula relative to the underly-
ing tissues.
The largest series of limited macular translocation by
Pieramici et al., in a retrospective review, analyzed the
outcome of 102 consecutive eyes of 101 patients that
underwent inferior limited macular translocation for
AMD-related subfoveal CNV. At three and six months
postoperatively, 37% and 48% of the eyes, respectively,
experienced ≥ 2 Snellen lines of visual improvement
(27)
.
After one year of follow-up, 39.5% still maintained a ≥ 2
lines of improvement, while 29.0% remained unchanged
and 31.4% lost ≥ 2 lines of visual acuity
(28)
. Recurrent
CNV developed in 34.6% of the eyes, being subfoveal in
most of the cases (65%)
(28)
.
Besides the usual risks inherent to pars plana vitrectomy,
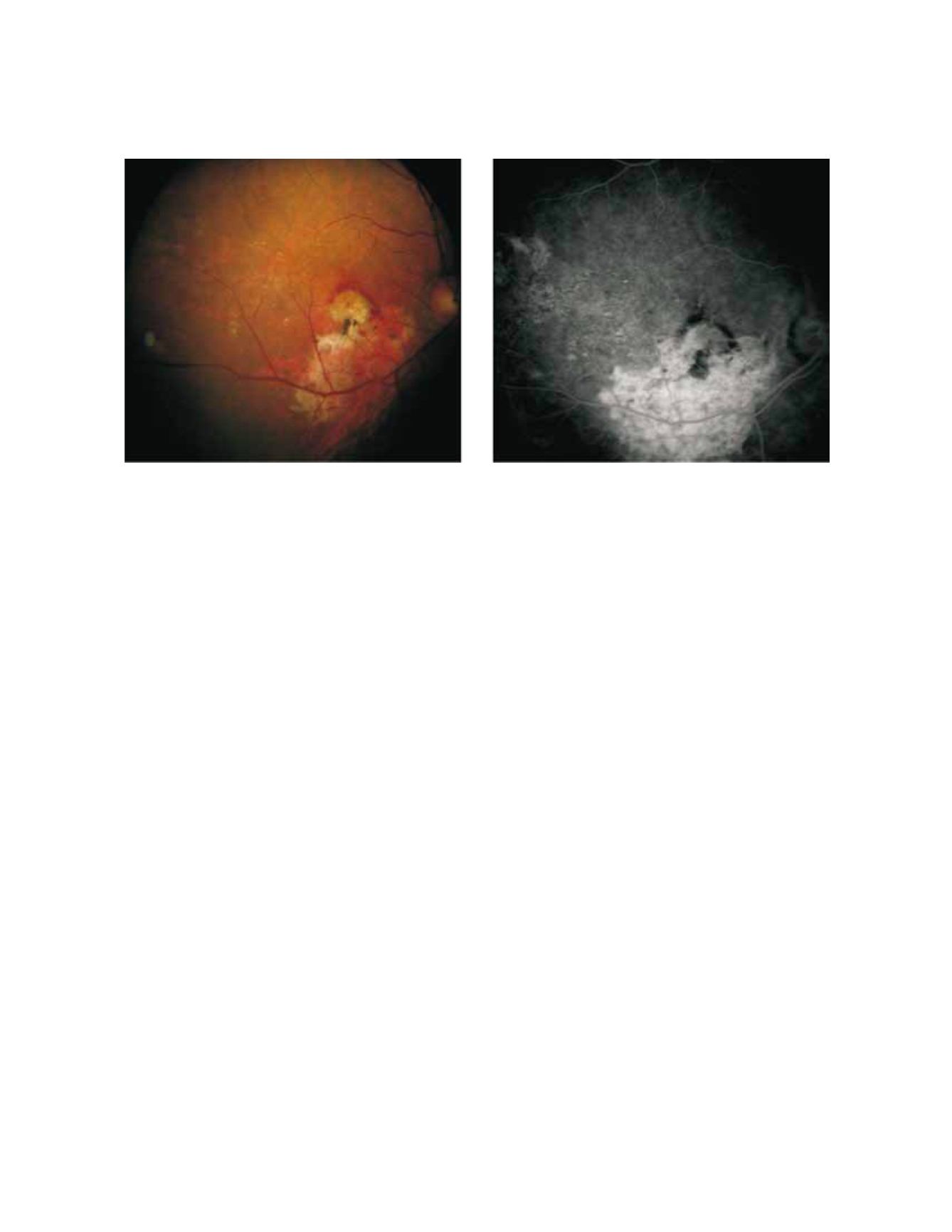
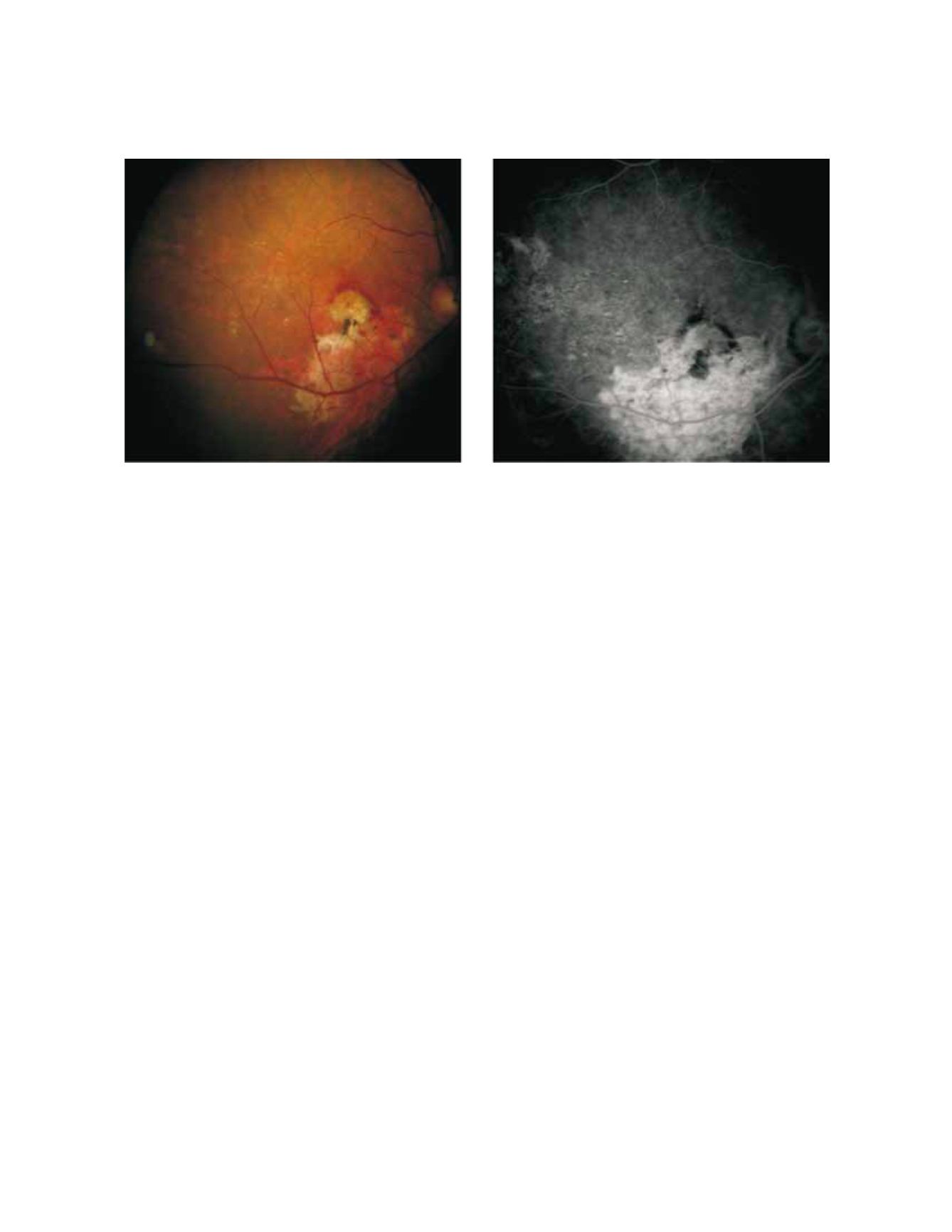
Figure 4 - Case II - A recurrent subfoveal CNV developed after the first year of follow-up, and the patient was started with intravitreal ranibizumab
injections. After 4 treatments, a visual acuity of 20/63 remained stable.