147
Serous PED
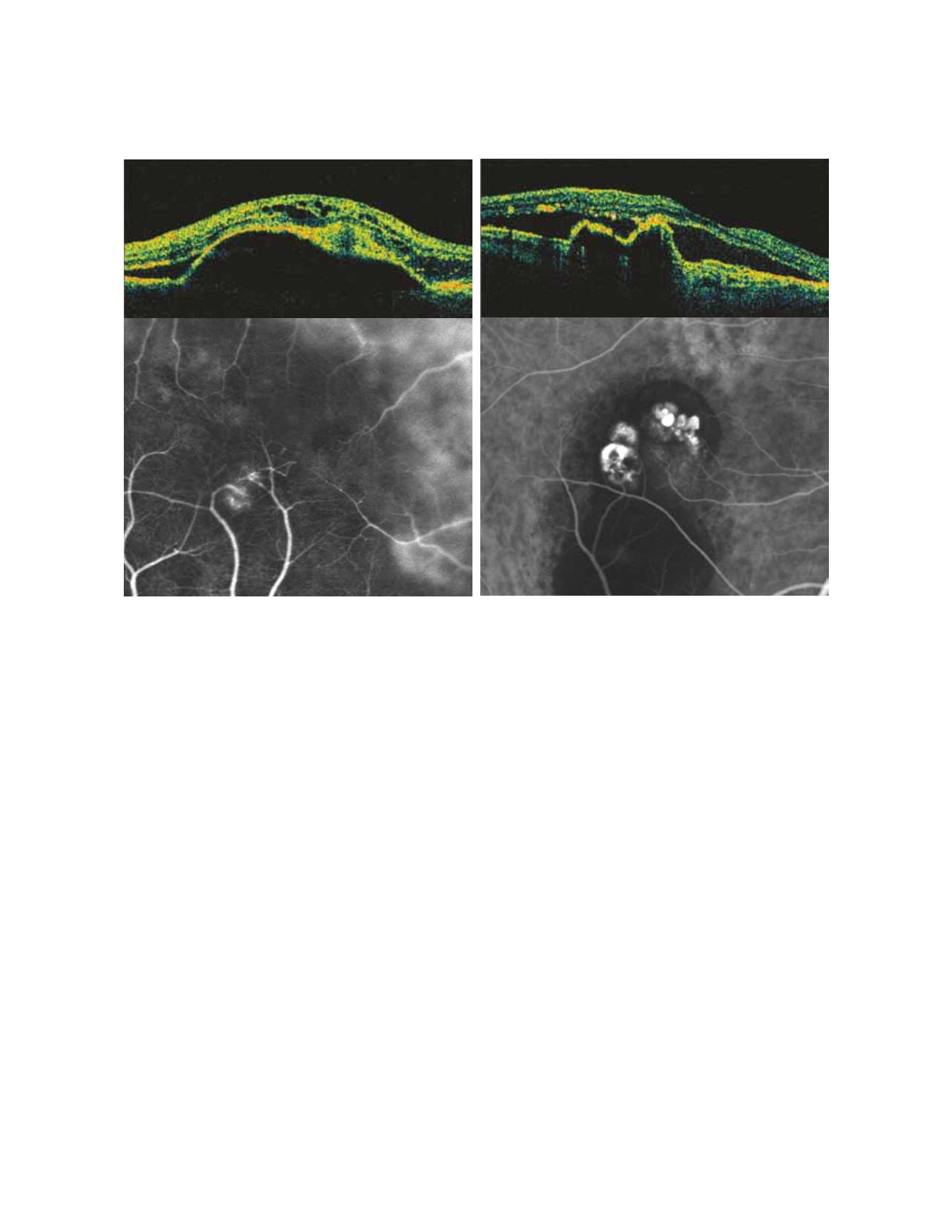
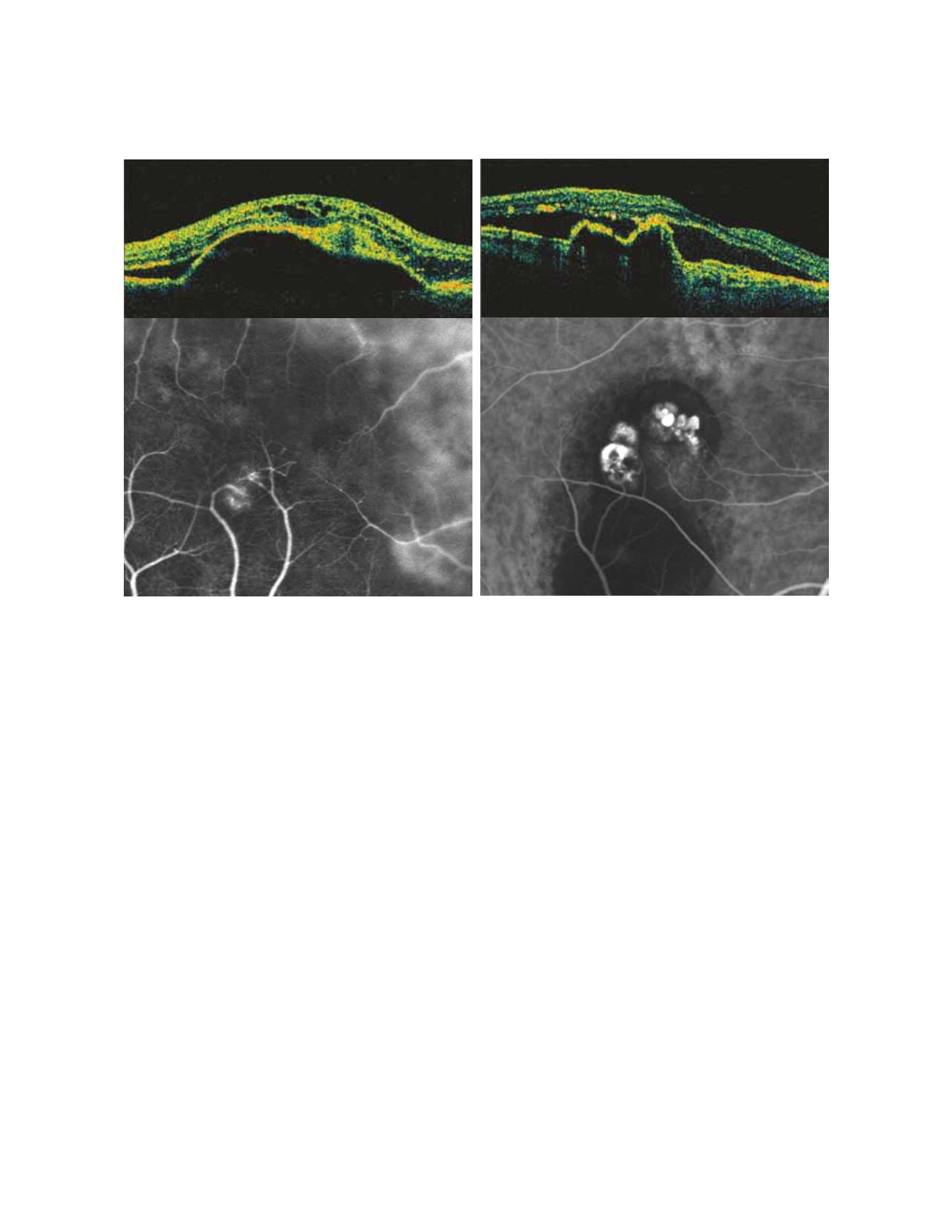
Figure 4 - Retinal Angiomatous Proliferation (right) and Polypoidal Choroidal Vasculopathy (left): ICGA and OCT patterns
been reported, varying from the heat generated by pho-
tocoagulation, to an abrupt increase of intra-PED fluid,
a contraction of the associated CNV or the concomitant
sudden resolution of the sub RPE fluid. The combining
presence of a vitreomacular traction and the deforma-
tion of the globe due to the mechanical trauma by the
needle have also been reported as causative agents
(58)
.
After RPE rips, the majority of patients complain a sud-
den severe visual decrease. In a small percentage of eyes,
where the tear spares the fovea, patients can even experi-
ence a temporary preservation of good visual function
(59)
.
However, in the long term, the progression of a subreti-
nal scar leads to a severe visual decrease. In the prognosis
of serous PED, it must be also considered the high risk
of bilaterality, with symmetrical behavior
(60)
.
Treatment of serous PED, associated or not with CNV,
has always been a challenge and so far there are no rec-
ommended guidelines for their management. Pure serous
PEDs have been treated in the past with laser grid or scat-
tered photocoagulation, nevertheless with disappointing
results
(61)
. No other approaches have been attempted to
treat these lesions. On the other hand, when a neovas-
cular net is present, treatment of serous PED has been
focused on CNVs management. However, given that
vascularized PEDs have never been included in the major
RCTs, we must establish our treatment decision on pub-
lished small series, often retrospective, that hint different
therapeutic approaches. By and large, in the antiangio-
genic therapy era, all the previous employed treatments
appear unsatisfactory to the occasion. Laser photocoagu-
lation, far-back widely employed, can still have a limited
indication when an ICG-well defined CNV lies remote
to the detached RPE
(62)
. Verteporfin photodynamic ther-
apy alone has been proved to be harmful, increasing the
risk of RPE tear, hemorrhages and sudden visual acuity
decrease
(43, 48, 49, 63)
(Fig. 5).
On the contrary, PDT combined with intravitreal tri-
amcinolone acetonide injection has been demonstrated
as potentially capable of visual acuity stabilization and
recurrences reduction
(64)
. However, the high rate com-
plications (cataract and glaucoma) has reduced the
intravitreal triamcinolone use. The optimistic results
obtained with the anti-VEGF intravitreal therapy in the
treatment of occult CNV have extended its employment
to the vascularized PED, however with disappointing
results
(65-68)
. As a matter of fact, both acute complications
A
B