183
Anti-VEGF in the treatment of AMD
colorectal and non-small-cell lung cancer, both approved
indications for this agent. Nevertheless, the intravitre-
ous administration of anti-VEGF agents for the treat-
ment of exudative AMD results in much lower systemic
exposures
(65)
.
Although the theoretical superior safety of pegaptanip in
comparison to other non‐selective anti‐VEGFs this has
not been confirmed yet.
5. Bevacizumab (Avastin®)
5.1 Introduction
Bevacizumab (Avastin
®
, Genentech, Roche) is a recom-
binant, humanized, monoclonal immunoglobulin G1
antibody (149 kD) that binds to and inhibits the biologic
activity of all isoforms of human VEGF. This molecule
has 2 antigen-binding domains (ranibizumab has 1). In
2004, the FDA approved bevacizumab for use in patients
with metastatic colorectal cancer. It has received additional
approval for use in patients with non–small-cell lung can-
cer and those with metastatic breast cancer
(78-81)
.
Though not formally studied or approved for any intraoc-
ular disease, Rosenfeld
’
s pioneering work and the unavail-
ability of a related ocular drug, ranibizumab, led to rapid
and wide use of bevacizumab all over the world
(82, 83)
.
Using bevacizumab as an intravitreal injection to treat
neovascular AMD is off-label at this time, however many
ophthalmologists, appropriately offer intravitreal beva-
cizumab to AMD patients based on multiple forms of
evidence: results from several retrospective case series,
extrapolation from the magnitude of the outcomes
reported with ranibizumab, the structural similarity
between ranibizumab and bevacizumab, the individual,
and the natural history of the disease if left untreated
(84)
.
In the human retina, it is unclear if the molecule of beva-
cizumab fully distributes within the retinal layers or if
localized inhibition of VEGF in the vitreous and inner
retina is responsible for the clinical effects associated with
administration
(85-87)
.
There are also theories that the larger size of bevacizumab
relative to ranibizumab may result in bevacizumab not
clearing as quickly from the eye, potentially resulting
in longer duration of activity. To the knowledge of this
author, this claim has not been confirmed
(84)
.
Full antibodies generally have longer systemic half-lives
than antibody fragments. Therefore, it is assumed that
the half-life of bevacizumab in the eye and in the circula-
tion is longer than that of ranibizumab after intravitreal
injection. Different half-lives for these 2 drugs may have
implications for different dosing frequencies and differ-
ent systemic toxicities
(78, 86-91)
.
5.2 Experimental and clinical studies
Following the initial successful administration of this
drug in the management of exudative AMD in May
2005, numerous case series were published illustrating
the effectiveness of this treatment in a high proportion of
patients
(92)
.
Almost all of the evidence supporting the use on neovascu-
lar AMD comes from off-label usage in short-term uncon-
trolled clinical case series, which suggests that intravitreal
administration is apparently locally and systemically well
tolerated and is associated with vision stabilization or
improvement in most treated eyes
(85, 86, 87, 91, 94)
.
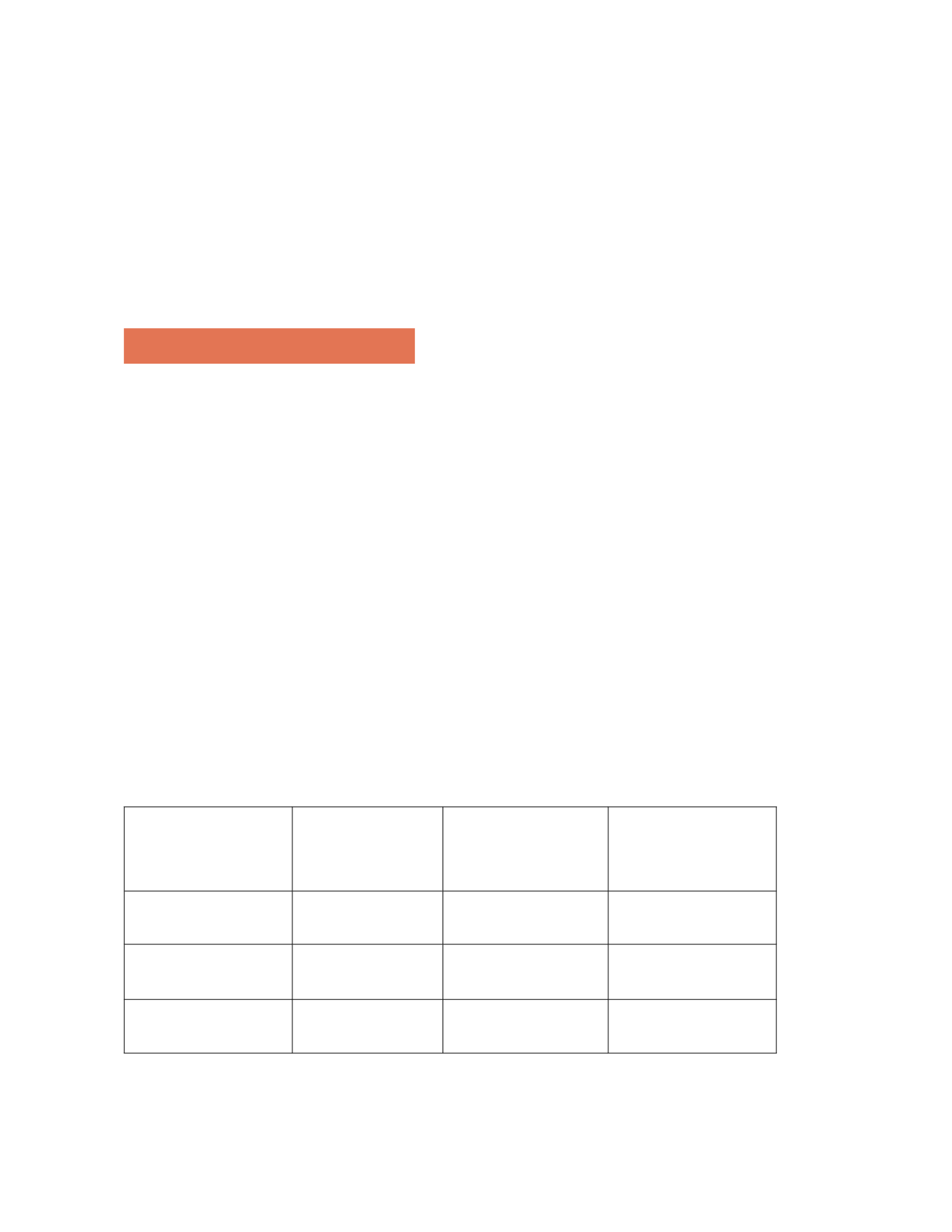
One of the earlier large retrospective case series in the
Event
Year 1
n = 7545 injections
Year 2
n = 4091 injections
Year 3
n = 3227 injections
Endophthalmitis
0.16
0.10
0.06
Traumatic cataract
0.07
0.02
0
Retinal detachment
0.08
0.17
0.03
Table 1 – VISION study serious ocular adverse events rates (% per injection)
61
. Adapted from Rajendra S Apte, 2008.