192
process and angiogenesis regulation.
The complexity and diversity of glucocorticoid (GC)
receptors in human tissue is highlighted by evidence
that up to 6,000 genes are expressed or suppressed
within hours of GC exposure. The enormous potential
of using exogenous GC agents to downregulate processes
involved in age-related macular degeneration must be
balanced against a similar potential for counterproduc-
tive effects
(9)
.
Steroids activate receptors that induce the synthesis of
specific proteins from DNA. Various mechanisms of
action are proposed for steroids.
It is known that steroids act on local inflammatory
mediators, stabilizing blood-retinal barrier function by
increasing gap junction density and activity in capillary
endothelial cells.
It is thought that triamcinolone decreases VEGF, which
is a potent agent in increasing capillary permeability by
increasing phosphorylation of proteins involved in tight
intercellular junctions, such as occludin and Zonula
Occludens-1 (ZO-1).
These agents also have an anti-inflammatory effect by
inhibiting phospholipase A2, an enzyme that metabo-
lizes cell membrane phospholipids to free arachidonic
acid, which, in turn, originates thromboxane, leukot-
Due to their synergistic effect, combined treatments
potentially lead to a decrease in the number of retreat-
ment sessions, as well as sustained long-term visual ben-
efits
(1)
, with gains and better clinical efficiency.
3. Synergistic action and increased
treatment effect
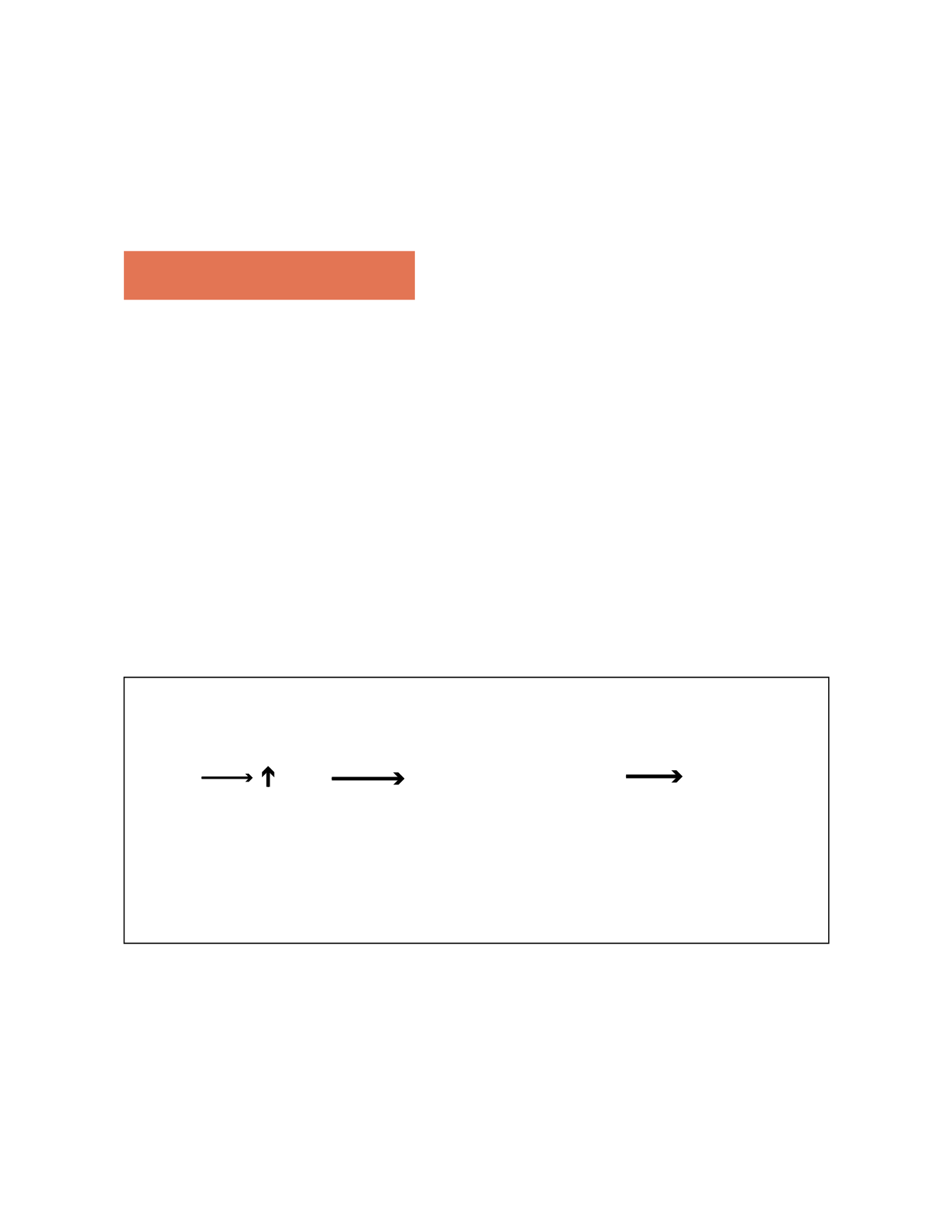
How can we explain the fact that a synergistic effect is
theoretically achieved by using various mechanisms of
action, sometimes more effective than the sum of their
separate effects? (Fig.1)
3.1 Anti-VEGFs
The primary need to act on the key mechanism of the
neovascularization process – VEGF – is widely known.
By acting on this mechanism not only do we inhibit neo-
vascularization but also act on oedema and the inflam-
matory mechanism, to a certain extent
(8)
.
3.2 Synergistic action of corticoids
When steroids are added, a synergistic action is achieved,
since steroids act on various levels of the inflammatory
Figure 1- Angiogenesis - New blood vessels are formed in response to various physiological and/or pathological stimuli, of which hypoxia, is one of
the most relevant. Hypoxia activates multiple cellular response cascades, with special emphasis on activation of extracellular matrix metalloproteases
and increased synthesis and release of growth factors, including VEGF. The latter acts on membrane receptors, activating intracellular enzyme
pathways through intracellular signalling, which results in response amplification. This ultimately leads to cellular proliferation, migration and dif-
ferentiation, with formation of new blood vessels. Different drug categories act on different stages of the neovascularization process
(6)
. Joint action on
various cascade levels should theoretically lead to an increase in treatment effect and/or a decrease in the effective dose and/or a more prolonged effect.
Hypoxia
VEGF
Anti-VEGF
Pegaptanib
Ranibizumab
Corticoids
Triamcinolone Acetate
PDT vertepor n
(angiothrombosis)
Intercellular and
Intracellular
pathways
activation
Proliferation
Migration
Proteolysis
New blood
vessels
{
//
//