131
Neovascular Phenotypes Polypoidal
recently with antiangiogenic drugs has precluded a bet-
ter knowledge of natural history of PCV with macular
involvement. Approximately half the patients with PCV
lesions in the posterior pole may have a favourable course
without treatment
(26)
. In the remaining half the disor-
der may persist for a long time with occasional repeated
bleeding and leakage, resulting in severe macular damage
and VA loss. Eyes with a cluster of grape-like polypoidal
dilations of the vessels may have a higher risk for severe
visual loss
(27,28)
.
Choroidal vascular lesions may be located in the peripap-
illary area, in central macula or in midperiphery. Most
of the PCV natural history series describe lesions in the
posterior pole, differentiating macular from extramacular
and/or peripapillary polyps
(5,7,28,29)
. Macular involvement
ranged from 25% to 94%. The analysis of VA outcome
must consider location of polyps and/or abnormal vascu-
lar network. Kwok et al.
(28)
followed the natural history
of nine eyes with macular involvement after a follow-up
ranging from 5 to 60 months and found VA improve-
ment of two lines in only one eye (11.1%), VA change of
one line in one eye, and VA decrease of two lines in seven
eyes (77.7%). Uhyama et al.
(26)
followed 14 eyes with
PCV (13 with macular involvement) for a mean period
of 39.9 months and described VA improvement of two
lines in five eyes (35.7%) and VA decrease of two lines in
four eyes (28.5%). A favorable course was demonstrated
in 50% of the cases with the remaining half of the cases
showing recurrent leakage and hemorrhages and progres-
sive VA loss.
Lesions may grow by enlargement with proliferation and
hypertrophy of the vascular component but, apparently
not by confluence. Polyps may bleed, grow, regress or
leak and a choroidal neovascularization may appear. A
massive spontaneous choroidal hemorrhage is rare but
may constitute a severe complication associated with
blindness
(27)
. Progression to RPE atrophy is common and
may be related with resolution of PED, chronic or recur-
rent leakage with PE or neurosensory detachment, auto-
infarction, regression or flattening of the lesion. Chronic
atrophy and foveal cystic degeneration is associated with
severe VA loss
(2,4,10,17,18,19,29)
.
5. Diagnosis
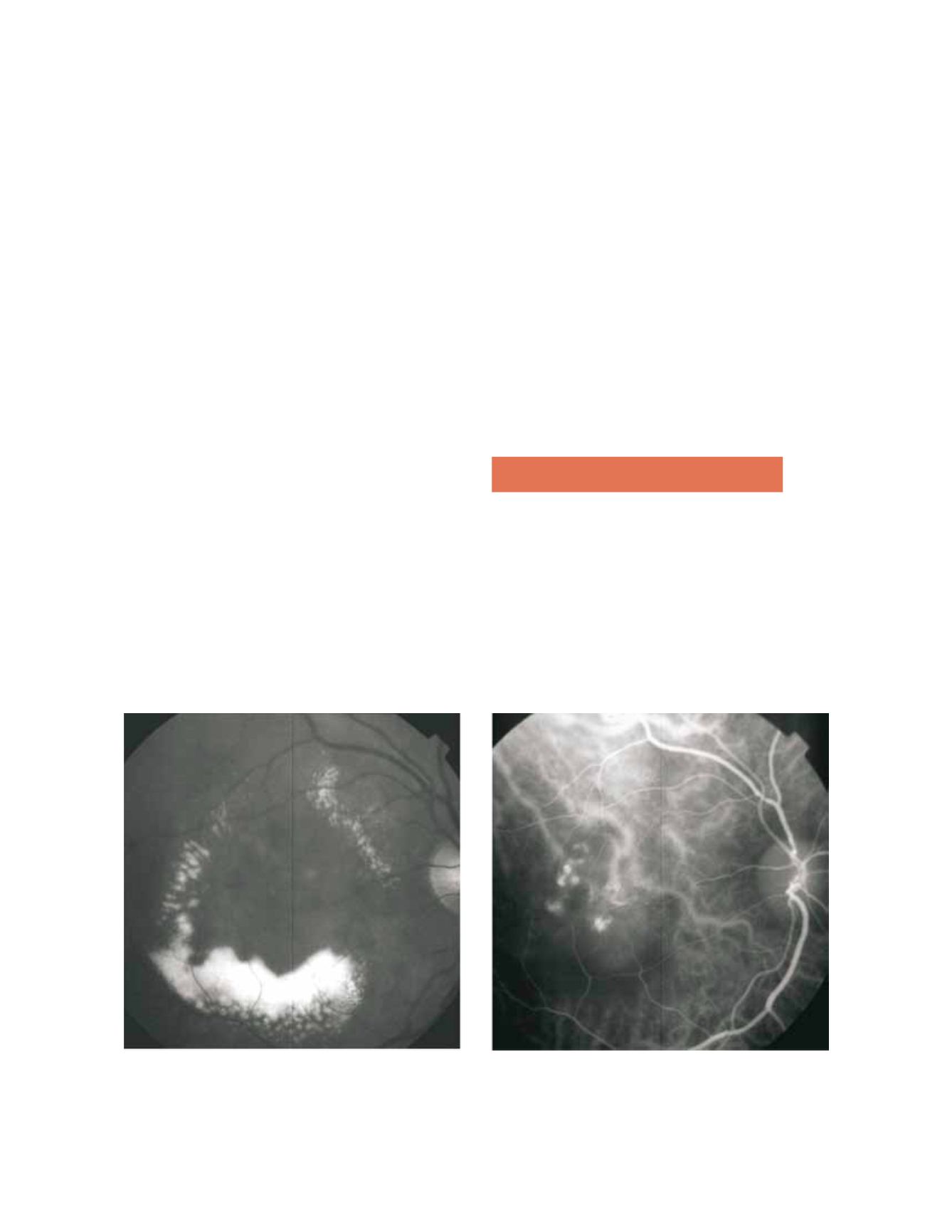
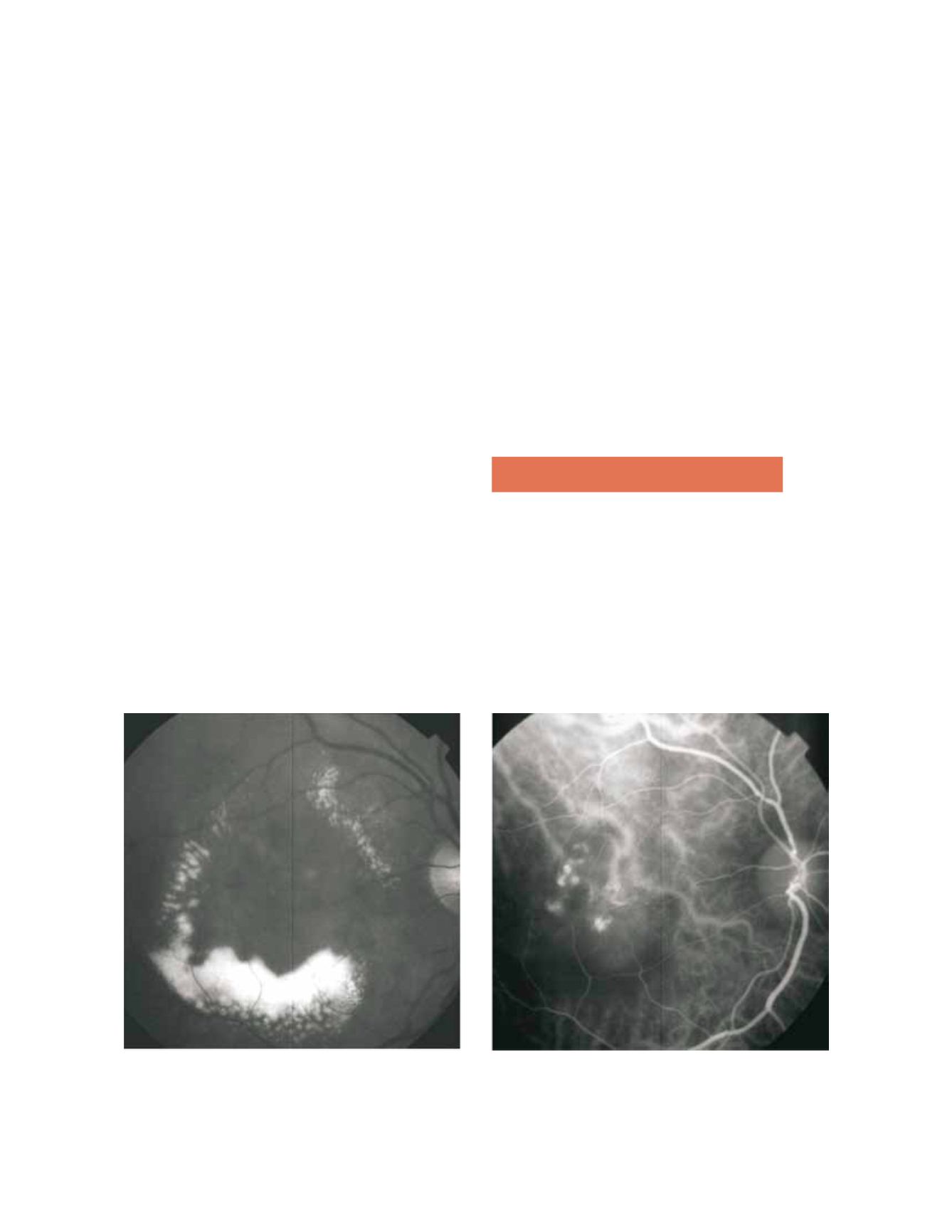
The diagnosis of PCV is based on ICG imaging (Fig. 1)
and may be complemented with OCT, fluorescein angi-
ography and fundus findings (Fig. 2, 3, 4).
Clinical examination may show one or more redish-
orange, spheroid, subretinal mass located at the macular
or juxtapapillary area (Fig. 2). This mass may correspond
to the anteriorly projection of multiple polyps and is very
suggestive of PCV. Also very suggestive of PCV is the
Figure 1. Polypoidal choroidal vasculopathy. Red-free (A) image with circinate lipidic exudation. Intermediate phase ICG shows an abnormal
choroidal vascular network and multiple polyps in the centre of the circinate exudation.
A
B