123
translocation surgery in eyes studied with FA and ICG.
The deep vascular anomalous complex was located in
front of the RPE, thus not representing choroidal
neovascularization. Nodular fibrovascular complexes
surrounded by a ring of diffuse drusen – basal linear
deposits under electron microscopy –, pigment epithe-
lium and an amorphous fibrous material containing
photoreceptor outer segment debris were observed.
The lesion was not covered by pigment epithelium;
however, the latter was preserved around the lesion.
The amorphous material did not cover the retinal
surface of the membrane, which adhered directly to
the outer nuclear layer in 50% of cases. Anastomoses
between fibrovascular nodules and the choroidal cir-
culation were only observed in cases showing isolated
disciform scars. Avascular fibrocellular membranes
were observed on the inside of Bruch’s membrane and,
in three cases, on the choroidal side of diffuse drusen.
Fibrin was present in affected retinas; choroidal anas-
tomosis was not observed. However, the latter possi-
bility was not excluded, since the specimens studied
may not have included the entire lesion. Serous PED
without CNV was observed in three cases.
Gass et al.
(13)
described chorioretinal anastomosis and
atrophy of the outer nuclear layer in a pre-clinical
case, with outer retinal capillaries moving close to a
choroidal neovascularization focus, having proposed a
choroidal origin for RAP, instead of the retinal origin
proposed by Yannuzzi.
In a histopathological study performed in nine neovas-
cular lesions classed as RAP, Shimada et al.
(29)
found
only intraretinal neovascularization in stage 2 cases. In
stage 3 cases, these authors found choroidal and intra-
retinal neovascularization; they concluded that their
findings were in agreement with the classification pro-
posed by Yannuzzi. These authors observed expression
of VEGF (in intraretinal neovascularization and in the
RPE), CD68-positive macrophages (in the neovascu-
larization area) and expression of hypoxia-inducing
factors alpha 1 and alpha 2 (HIF 1 alpha and 2 alpha)
in neovascular endothelial cells. According to these
authors, intraretinal neovascularization would appear
before the occurrence of choroidal neovascularization
and be associated with ischemia and increased expres-
sion of VEGF and inflammatory factors.
Monson et al.
(30)
described the histopathological char-
acteristics of RAP in an 87-year-old woman. The images
obtained by fundus examination and fluorescein angi-
ography were histopathologically consistent with a
neovascular intraretinal angiomatous complex without
significant VA loss was observed in 69% of eyes and vision
did not improve in any case
(14)
. Significant loss of vision
was observed in the first 3 months after diagnosis; a trend
towards stabilization was observed subsequently, with no
significant differences in average VA being observed at 3, 6
and 12 months and at the end of the study (p>0.05).
Viola et al.
(24)
obtained also poor results: in 81% of cases,
visual acuity had decreased by 2 ETDRS lines or worse by
occasion of the 6-month examination. On final examina-
tion (6 - 44 months), 62% of study subjects showed subret-
inal fibrosis, with 56% showing chorioretinal anastomosis.
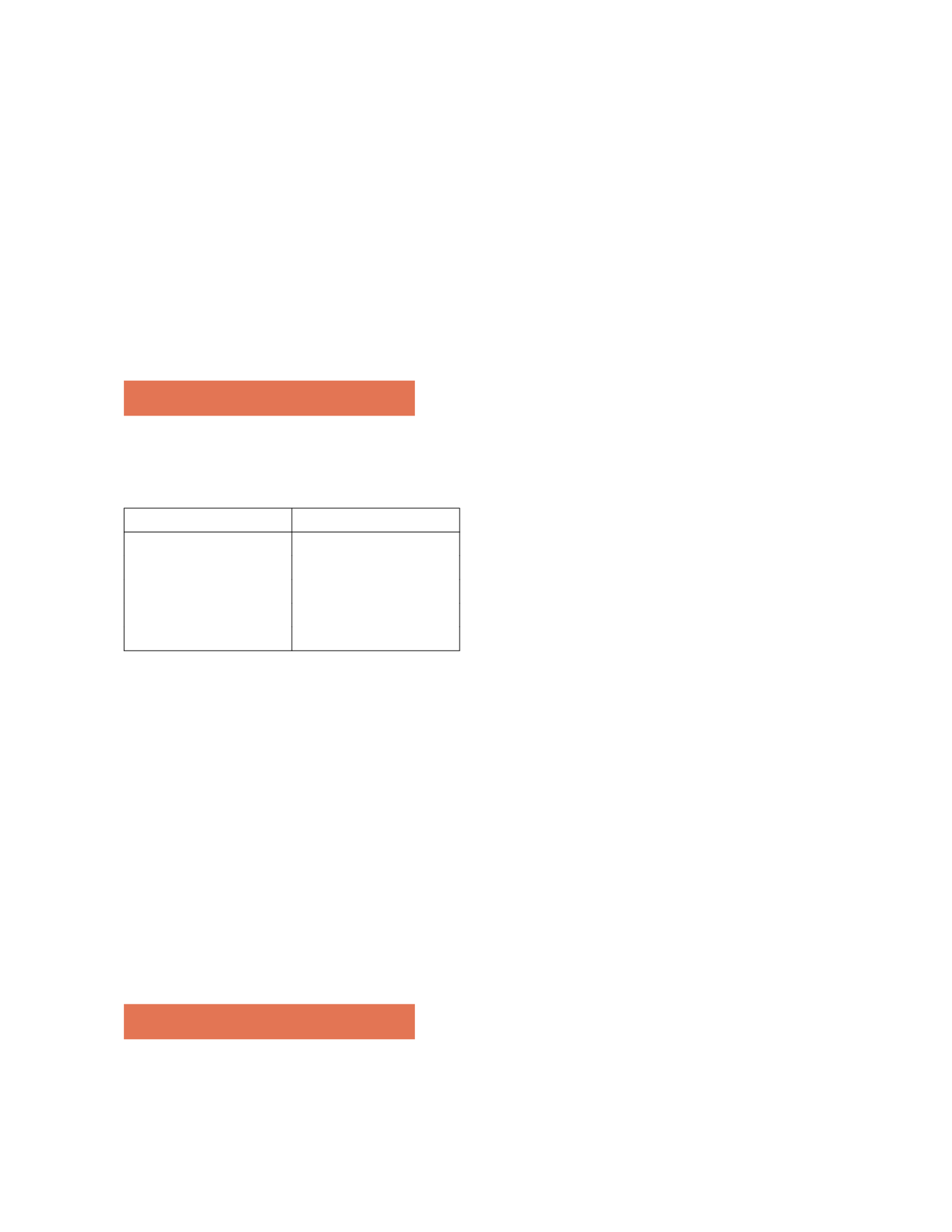
6. Epidemiology
RAP was observed in 5 to 28% of new cases of occult exu-
dative neovascularization (Table 1).
Table 1: Percentage of RAP
Country-Year
Percentage
France (1995)
(13)
26.8%
Israel (2002)
(20)
28%
USA (2002)
(26)
5%
Portugal (2004)
(15)
9.4%
Italy (2008)
(27)
25%
Kuhn et al.
(12)
and Axer-Siegel et al.
(19)
used SLO angiogra-
phy, while Fernandes et al.
(25)
used videoangiography, which
may explain the differences observed. Using the ImageNet
1024 videoangiography system, our team observed a preva-
lence of 9.4% in a consecutive series of 563 patients
(14)
.
Women appear to be more affected, corresponding from
64.7% to 71% of patients
(8,12)
.
Patients with RAP are normally older than those show-
ing occult membranes or membranes with classic compo-
nents – average age of 79 vs. 76 years
(6,8,9)
. The average and
median ages of a series of 108 patients studied by Yannuzzi
et al.
(9)
were 80 and 81 years respectively. Both eyes were
similarly affected in 51.9% of patients, with RAP occur-
ring in the second eye an average 15 months after appear-
ing in the first eye. At 3 years, both eyes were affected in
100% of patients
(26,27)
. Prevalence appears to be greater in
hyperpigmented eyes
(8,9,28)
.
7. Anatomopathology
Lafaut et al.
(18)
studied six “deep retinal vascular
anomalous complex” lesion specimens from retinal
Neovascular Phenotypes: RAP (Retinal angiomatous proliferation)